A major new consortium led by University College London Hospitals NHS Foundation Trust (UCLH) and UCL, and supported by ARC North Thames, has recently been awarded £6.8 million by the National Institute of Health Research (NIHR) to conduct the largest clinical study of long COVID over the next two years.

As countries around the world struggle to cope and recover from successive waves of the COVID-19 pandemic, the research programme will inform medium- and longer-term policy and health system responses.
The consortium is made up of more than 30 researchers, health professionals, patients and industry partners from over 30 organisations working together under the banner of STIMULATE-ICP (Symptoms, Trajectory, Inequalities and Management: Understanding Long-COVID to Address and Transform Existing Integrated Care Pathways).
It is hoped that the programme will deliver knowledge to clinicians and scientists, evidence to policymakers, and improved care to patients, while collecting real-world data at scale. The team spans a wide range of relevant clinical and academic disciplines including primary care and specialist services, epidemiology, mental health and health economics. It also includes four patient groups who helped develop the research proposals.
The study is co-led by UCL and ARC key researcher Professor Amitava Banerjee, who is a professor of clinical data science at the UCL Institute of Health Informatics and consultant cardiologist at UCLH. Prof Banerjee said:
“Two million people in the UK are estimated to have had persistent symptoms for more than 12 weeks following initial COVID infection, with far-reaching impact on patients, healthcare and the economy.
“More than 80 long COVID clinics have been established around England but we need to better understand, diagnose and treat this new disease. Inequalities in access to and provision of long COVID care have already become apparent”.
To improve recovery, the team will work out what long COVID is, how to diagnose it and how to manage it. They will interview patients and health professionals and analyse data from NHS records, informing our understanding of patterns of long COVID and the outcomes of current clinical practice.
Co-lead Dr Melissa Heightman, a consultant in respiratory medicine who runs the UCLH post-Covid follow-up service, said:
“We established our post-COVID clinic in London in May 2020 during the peak of the first wave, ‘building the plane while we were flying it’ and based in the hospital through necessity.
Dr Heightman continued:
“Individuals with long COVID need integrated services, working across traditional healthcare boundaries to best meet their complex care and rehabilitation needs. The aim will be to deliver timely high-quality care close to peoples’ homes with community-based diagnostics but access to specialist input when needed.”
Within the overall programme of research, a trial coordinated by the University of Central Lancashire will recruit over 4,500 people with long-COVID, starting with six sites in Hull, Derby, Leicester, Liverpool, London (UCLH) and Exeter.
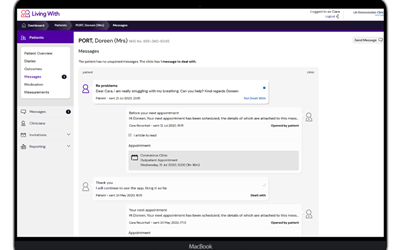
Individuals will be randomly assigned to usual care or a new pathway, including a community-based, comprehensive MRI scan (using imaging technology called CoverscanTM developed by Perspectum) which can map the effects of COVID-19 on several of the body’s key organs. They will also be given enhanced rehabilitation. using the ARC-supported digital health platform ‘Living with COVID Recovery’, which is led by UCL and ARC researcher Professor Elizabeth Murray.
Within this research programme, another trial will test different drugs, such as aspirin and colchicine, to measure effects of three months treatment on symptoms, mental health, return to work and other important outcomes. Researchers will also work alongside patients to co-develop ways of improving access to care and support, to address care inequalities.
Lyth Hishmeh, who has suffered with long COVID since the first wave of the pandemic, sees the benefit of research which considers all aspects of the patient pathway:
“Patients and health professionals faced and continue to face difficulties in knowing what to do for long COVID. A comprehensive study like STIMULATE-ICP is needed to look at the big picture and improve patient access to the right care at the right time in the right place.”
The STIMULATE-ICP consortium includes a number of partners and NIHR Applied Research Collaborations (ARCs) across the country including ARC North Thames, ARC South West Peninsula, ARC East Midlands, ARC Yorkshire and Humber, and ARC North West Coast.
STIMULATE-ICP is one of 15 new projects funded as part of a £19.6 million comprehensive package of new NIHR-funded research to help improve understanding of long COVID, from diagnosis and treatment through to rehabilitation and recovery. Find out more about the projects funded.
ABOUT STIMULATE-ICP
The STIMULATE-ICP consortium includes: UCLH, UCL, University of Central Lancashire, LongCovidSOS, UK Doctors #Longcovid, Royal College of General Practitioners, University of Liverpool, Liverpool University Hospitals Foundation Trust, Perspectum, Living With, University of Hull, Hull University Teaching Hospitals Trust, University of York, University of Leicester, University of Exeter, University of Southampton, University of Sussex, Alliance Medical, GE Healthcare, Olink, Francis Crick Institute, British Heart Foundation (BHF) Data Science Centre, BHF Data Science Centre, Health Data Research UK, Office of National Statistics, and Royal Devon and Exeter NHS Trust. It is supported by NIHR Applied Research Collaborations (ARCs) for the North Thames, South West Peninsula, East Midlands, Yorkshire and Humber, and North West Coast, as well as having NIHR Clinical Research Network support.

 19 Jul 2021
19 Jul 2021